CE / CME
ABIM MOC: maximum of 0.75 Medical Knowledge MOC point
Physicians: Maximum of 0.75 AMA PRA Category 1 Credit™
Released: September 16, 2025
Expiration: March 15, 2026
Introduction
In this module, Tanya B. Dorff, MD and Phillip H. Kuo, MD, PhD, FACR, discuss the current landscape in metastatic castration-resistant prostate cancer (mCRPC), including the present application of prostate-specific membrane antigen positron emission tomography /computed tomography (PSMA-PET/CT) for assessing patient eligibility for radioligand therapy and as a predictive marker of tumor response. Experts also discuss recent approvals and expanded indications for radioligand therapy and their recommendations for how to integrate these therapies into everyday clinical practice.
The key points discussed in this module are illustrated with thumbnails from the accompanying downloadable PowerPoint slideset, which can be found here or downloaded by clicking on any of the slide thumbnails in the module alongside the expert commentary.
Please note that Clinical Care Options (CCO) plans to measure the educational impact of this activity. Some questions will be asked twice: once at the beginning of the activity, and once again after the discussion that informs the best choice. Your responses will be aggregated for analysis, and your individual responses will not be shared. Thank you in advance for helping us assess the impact of this education.
Before continuing with this educational activity, please take a moment to answer the following questions.
Metastatic Castration-Resistant Prostate Cancer
Tanya B. Dorff, MD:
Metastatic CRPC remains incurable with approximately 63% of patients dying from their disease within 5 years of diagnosis.4
In this module, we will briefly discuss the clinical implications for the presentation of mCRPC, the available treatment options, and current unmet needs for patients in this disease setting. We will also focus more deeply on the available and emerging radioligand therapies options.
Clinical Course of Prostate Cancer
Tanya B. Dorff, MD:
Patients with prostate cancer may present with nonmetastatic prostate cancer that progresses to metastatic disease or with de novo metastatic prostate cancer—either hormone-sensitive metastatic prostate cancer or androgen deprivation therapy (ADT)–resistant mCRPC. The hormone-resistant form of prostate cancer is characterized by rising levels of PSA despite castrate levels of testosterone with ongoing ADT or following orchiectomy.5
This module will focus on mCRPC only, which is more likely to develop cancer-related symptomatic disease and comorbidities with an associated higher likelihood of disease mortality.6
Available Options for mCRPC
Tanya B. Dorff, MD:
Patients with mCRPC often stop responding to ADT therapy (eg, docetaxel with or without abiraterone or darolutamide, enzalutamide, apalutamide). Next-generation sequencing (NGS) is then used to help identify appropriate next best treatment options. NGS testing results may identify BRCA mutations (germline or somatic) or homologous recombination repair (HRR) pathway alterations (Palb2), which in turn inform selection of PARP inhibitors (olaparib, niraparib, rucaparib, or talazoparib).7 Alternatively, identification of microsatellite instability–high (MSI-H), mismatch-repair deficient (dMMR), or high tumor mutational burden can also inform the tumor agnostic use of immune-checkpoint inhibitor pembrolizumab.8
However, actionable mutations are only found in a small fraction of patients,9,10 and mCRPC lacking actionable biomarkers may receive guideline recommended ARPI or chemotherapeutic agents such as docetaxel or cabazitaxel.5,7 Patients with asymptomatic or minimally symptomatic mCRPC may also have the option to receive sipuleucel-T, an autologous cellular immunotherapy vaccine that uses the patient’s immune system to fight the cancer.11,12 Moreover, in patients without actionable biomarkers who progress on ARPI with or without previous docetaxel, now we have access to radioligand therapy options and these will be the main focus of this module.3,13
Phillip H. Kuo, MD, PhD, FACR:
In 2025, patients have the choice of pursuing radioligand therapy earlier in the treatment course, which has created a need for more education on this topic. Radioligand therapy options are an attractive tool in the treatment of mCRPC, particularly if bone metastases are present and for sites that present with detectable/significant levels of PSMA-positivity in tumor cells.
mCRPC: Unmet Needs and Current Status
Tanya B. Dorff, MD:
A persistent unmet need in patients with mCRPC is the fact of disease recurrence. This is often a consideration when ensuring that we offer patients all available therapeutic options with the potential for prolonging survival. As we are counseling patients about the therapeutic choices available to them, we often take into consideration the level of androgen therapy refractoriness and/or previous use of docetaxel, but also the pace of disease progression and the sites of metastases. I would also note that there are differences in disease prognosis based on the location of the metastatic site for mCRPC. For instance, patients who have lymph node–only metastasis have a longer OS (31.6 months) compared with patients who have liver metastasis (13.5 months).14
Characteristics of Cell Surface Targets
Tanya B. Dorff, MD:
The need for improved imaging and therapeutics options in patients with mCRPC led to exploring the targeting of PSMA to enable specific delivery of anticancer therapy that was more selective for malignant prostate cancer cells.
Benefits of PSMA cell-surface antigen targeting in mCRPC detection and treatment include15:
All of these favorable features for targeting PSMA have led to the development of several research programs including for radioligand-based approaches for targeting the PSMA receptor on the surface of prostate cancer cells.16
FDA-Approved Radioligand Therapies in mCRPC
Tanya B. Dorff, MD:
At the present time, there are 2 FDA-approved radiopharmaceutical therapy options available in the United States for patients with mCRPC.
The first approved radiopharmaceutical therapy for mCRPC was radium-223 dichloride (or radium-223), an alpha particle emitter that was approved in 2013 for patients with mCRPC with bone metastases and no known visceral metastases present.13
The second radiopharmaceutical therapy option is 177Lu-PSMA-617. Approved in 2022, 177Lu-PSMA-617 became the first PSMA–targeted radiopharmaceutical therapy for patients who had received previous ARPI and taxane-based chemotherapy.3 More recently, 177Lu-PSMA-617 received an expanded indication to include patients who have previously undergone treatment with ARPI therapy and are suitable candidates for delaying taxane-based chemotherapy.
Radium-223: Pharmacology and Other Considerations
Tanya B. Dorff, MD:
Radium-223 is dosed at 55 kBq (1.49 microcurie)/kg body weight every 4 weeks for a total of 6 injections.13 In general, radium-223 can distribute across the gastrointestinal tract, liver, lungs, kidneys, heart wall, bone marrow, and salivary glands. Consequently, radium-223 can be absorbed by unintended organs such as bone marrow and digestive system, which may result in adverse events (AEs) occurring in these tissues.
Because of radium-223 distribution patterns, patients must be monitored for anemia, cytopenias (lymphocytopenia, leukopenia, thrombocytopenia), nausea, diarrhea, vomiting, neutropenia, and peripheral edema.
Additional safety considerations include following institutional policies regarding the handling and exposure to radioactive agents including use of personal protective equipment (PPE) and safety screens when appropriate.
Although not listed in the prescribing information, I consider a hemoglobin level less than 9.0 g/dL to be a relative contraindication for using radium-223. In addition, exhibiting a “superscan” that may be associated with marrow toxicity.
Phillip H. Kuo, MD, PhD, FACR:
In my experience, radium-223 is a generally well-tolerated drug. Also when considering a patient for radium-223, a hemoglobin less than 9.0 g/dL might certainly give me pause, but it is not an absolute contraindication for whether or not the patient qualifies for this therapy. Other things that I might consider to be relative contraindications might be cytopenias such as thrombocytopenia, and to a lesser extent neutropenia.
Radium-223: Mechanism of Action
Tanya B. Dorff, MD:
Radium-223 is a calcium mimic that works by binding into new abnormal bone formations associated with mCRPC bone metastases.17 Once bound to hydroxyapatite and incorporated into bone-associated prostate cancer metastases, radium-223 releases 4 alpha particles for every atom which in turn promote double-stranded breaks in DNA. The short-range linear effects of the alpha particles emitted by radium-223 result in a shorter-range cell killing and favorable sparing of normal bone structures vs metastatic prostate cancer cells.
Phillip H. Kuo, MD, PhD, FACR:
Radium is chemically similar to calcium and thus incorporates into the inorganic boney matrix, a very different mechanism from the typical cellular-targeted therapies. Therefore, the familiar nuclear medicine bone scan provides an important imaging biomarker to assure good uptake of radium at the site of bone metastases, since the imaging radiopharmaceutical has a similar mechanism of uptake as radium-223.
In my experience, radium-223 is rarely discontinued due to side effects. Instead, the drug is more often discontinued due to disease progression. It also should be noted that serum PSA is not a good marker to track for response and PSMA-PET, CT, or MRI must be used to evaluate for soft tissue disease progression if PSA is rising during radium-223 treatment.
177Lu-PSMA-617: Pharmacology and Other Considerations
Tanya B. Dorff, MD:
According to the prescribing information, 177Lu-PSMA-617 is prepared from a single-dose vial (1000 MBq/mL [27 mCi/mL]) used for intravenous administration.3 The recommended treatment dose is 7.4 GBq (200 mCi/mL) given intravenously every 6 weeks for 6 doses. Of note, radiation exposure from 177Lu-PSMA-617 may increase in patients with a certain degree of renal impairment (CrCl 30 mL/min-50 mL/min).
We can often minimize exposure to normal tissues particularly the kidneys and urinary bladder by asking the patient to increase fluid intake and to void as often as possible. Other considerations for minimizing exposure to other individual bystander and family members include social distancing (≥3 feet) for at least 2-3 days (approximately 7 days for children and pregnant women). The prescribing information suggests sleeping in separate rooms from children for 7 days or pregnant women for 15 days.3
Patients with poor renal function (CrCl <50 mL/min) were not included in the in the clinical trials supporting the use of 177Lu-PSMA-617 (NCT03511664). However, I consider select patients with CrCl <50 mL/min who may be candidates for 177Lu-PSMA-617 if no unresolvable kidney obstructions, not on hemodialysis, and if they do not have a very low glomerular filtration rate of <30 mL/min.
Before receiving this 177Lu-PSMA-617, we should educate patients about the signs and symptoms of anemia (eg, fatigue, weakness, pale skin, shortness of breath, easier bruising or bleeding), and about management of dry mouth to avoid consequences such as dental cavities, anorexia/weight loss.
Similar to radium-223, safety considerations for handling 177Lu-PSMA-617 include following institutional policies regarding radioactive agent use in nuclear medicine and use of PPE and safety screens.
Phillip H. Kuo, MD, PhD, FACR:
177Lu-PSMA-617 is predominantly cleared by the kidneys and patients with decreased renal function may potentially have the drug stay in their body longer, resulting in a greater exposure of radiation to normal tissues, particularly the bone marrow, than in patients without renal impairment. I also do not consider a mildly impaired renal function to be an absolute contraindication to receiving this therapy. We must always weigh the risks and benefits of all therapies and we often proceed in patients with mild comorbidities because the benefits of radioligand therapy outweigh the risks.
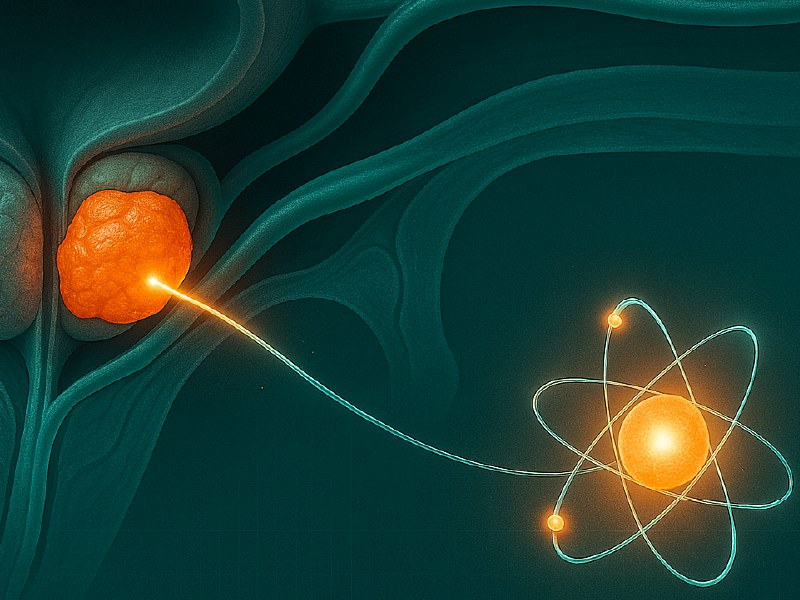
177Lu-PSMA-617–Targeted Radioligand Therapy
Tanya B. Dorff, MD:
177Lu-PSMA-617 works by targeting the PSMA transmembrane protein on the surface of prostate cancer cells and upon binding to the PSMA receptor it causes internalization of the complex via endocytosis.1 8 The internalized radioligand (Lutetium 177), which is linked to PSMA, delivers beta particle radiation to the target cell which leads to double-stranded DNA damage and cell death.
Visual Estimation of PSMA+ Status in mCRPC
Basis of PSMA PET/CT Use as a Companion Diagnostic in mCRPC
Phillip H. Kuo, MD, PhD, FACR:
Patients must be qualified for 177Lu-PSMA-617 radioligand treatment using a diagnostic radiotracer and PET/CT scanning to assess the level of PSMA-expression on metastatic prostate cancer lesions throughout the body. This method can also be used to monitor the status of radioligand target lesions during and after treatment.3,19
To properly select patients for 177Lu-PSMA-617, we currently use visual assessment of PSMA PET/CT. We may use a score of 0, 1, 2, or 3 for uptake-avid lesions. PSMA-positive is visually greater than liver, while PSMA-negative is visually the same or less than liver. PSMA-positive and PSMA-negative in this setting is not about whether the lesion is a prostate cancer. We are assessing the PSMA uptake of prostate tumors/metastases for the purpose of eligibility for 177Lu-PSMA-617. If the lesion has an uptake value that is equal to or lower than the blood pool, it receives a score of 0. If the lesion has an uptake value equal to or lower than liver but higher than blood pool it receives a score of 1. If the lesion has an uptake value higher than liver and equal to or lower than parotid gland or higher than parotid gland it receives a score of 2 or 3, respectively.1 Lesions scoring 2 or higher are regarded as PSMA-positive and patient is deemed eligible for radioligand therapy based on this visual PET/CT assessment. Just as or even more important and more challenging than identifying at least one site of PSMA-positive disease is identifying PSMA-negative tumors.
Tanya B. Dorff, MD:
The PSMA PET/CT procedure has a high degree of sensitivity and is much better at assessing tumor burden than PSA testing alone. With PSMA PET/CT assays we can:
Of importance, 20% to 50% of patients with prostate cancer will experience biochemical recurrence following definitive therapy.20,21 In this setting, it is well established to perform metastasis-directed radiation and oligometastatic disease–directed radiation and we are using PET scans to accomplish this as well.
Although most of us can perform these types of scans quite readily in standard practice, there can be challenges regarding access and insurance authorization. In California where I practice, we have favorable coverage for prostate cancer through Medicare. In general, we can obtain PSMA PET/CT and insurance approval when being used to select a patient for 177Lu-PSMA-617.
Selecting Patients for PSMA-Targeted Therapy: VISION Trial Criteria
Phillip H. Kuo, MD, PhD, FACR:
As a reminder, the FDA selection rules for 177Lu-PSMA-617 were based on the phase III VISION trial2 that evaluated use of 177Lu-PSMA-617 vs protocol-defined standard of care (SoC) (ie, excluding chemotherapy, systemic radioisotope, immunotherapy, and investigational drugs) in patients with PSMA-positive mCRPC and ≥1 prior ARPI and prior ≥1 taxane. The selection criteria included first assessing to ensure at least one PSMA-positive lesions (defined as having an uptake greater than liver by visual assessment). Then assess for the presence of even one PSMA-negative lesion (defined as having uptake same or less than liver by visual assessment) that meets the size criteria (ie, lymph node ≥2.5 cm in short axis anywhere in the body; solid organ ≥1 cm in short axis; and bone metastases with soft tissue component ≥1 cm in short axis).22 In brief, if no PSMA-positive lesions were identified then patients would be excluded from consideration of PSMA-targeted radioligand therapy—this was a fairly unusual patient. The more common reason for exclusion was having one or more PSMA-negative lesions (≥1) lesions meeting the size threshold (ie, lymph node: ≥2.5 cm; solid organ ≥1 cm; bone metastases ≥1 cm). Importantly, a PSMA-negative node that is less than 2.5 cm in short axis would not exclude the patient from eligibility for 177Lu-PSMA-617.
Data in Support of Radium-223 Use in mCRPC
Tanya B. Dorff, MD:
Now that we have provided a comprehensive introduction to the treatment setting and the rationale for the use and mechanism of action of radioligand therapies such as radium-223 and 177Lu-PSMA-617, we will briefly highlight the data which support the current indications and touch on a few recent data updates.
ALSYMPCA: Efficacy of Radium-223 in mCRPC
Tanya B. Dorff, MD:
The randomised, double-blind, phase III ALSYMPCA trial evaluated radium-223 vs placebo 2:1 in patients with symptomatic mCRPC, with at least 2 symptomatic bone metastases, no known visceral metastases, and receiving best SoC, including those with previous docetaxel use and no previous docetaxel use (n = 921).23 ALSYMPCA showed that radium-223 improved OS compared with placebo in both the previous docetaxel (HR: 0.70; P = .01) and no previous docetaxel (HR: 0.69; P = .01) groups and was well tolerated in patients with mCRPC with symptomatic bone metastases, leading to its FDA approval in 2013.
I also found interesting the data showing there was a significantly prolonged median time to first symptomatic skeletal event with radium-223 vs placebo (15.6 vs 9.8 months; HR: 0.66; 95% CI: 0.52-0.83; P = .0004) and reduced time in the hospital.
PEACE-3: Enzalutamide ± Radium-223 in mCRPC
Tanya B. Dorff, MD:
More recently, the international, randomized, open-label, phase III PEACE-3 trial compared the efficacy and safety of adding radium-223 to enzalutamide vs treatment with enzalutamide alone in patients with confirmed prostate cancer and 4 or more bone metastases with or without lymph node involvement and who were either asymptomatic or mildly symptomatic and no central nervous system or visceral metastases. Patients previously treated with or concomitantly using CYP17 inhibitors were excluded, which I think is important to note.24,25 The primary endpoint of the study was rPFS.
PEACE-3: Fracture Rates by Mandating Use of BPAs With Enzalutamide ± Radium-223
Tanya B. Dorff, MD:
For patients receiving radium-223 plus enzalutamide in PEACE-3, early on we saw an increase in the cumulative incidence of fractures compared with enzalutamide alone (24.3% vs 13.4%). This highlighted a need of using bone protective agents (BPA; zoledronic acid or denosumab) and fortunately following implementation of BPAs in this trial we saw a dramatic reduction in bone fractures for both treatment arms. Most grade 3 treatment-emergent AEs were comparable between treatment arms.
PEACE-3: rPFS and OS
Tanya B. Dorff, MD:
Regarding the primary endpoint of rPFS and key secondary endpoint of OS, both were improved with the addition of radium-223 to enzalutamide. The median rPFS in the radium-223 plus enzalutamide arm was 19.4 months (95% CI: 17.1-25.3) compared with 16.4 months (95%CI: 13.8-19.2) with enzalutamide alone (HR: 0.69; 95% CI: 0.54-0.87; P = .0009).25 Similarly, median OS was prolonged in the combination arm at 42.3 months (95% CI: 36.8-49.1) compared with 35 months (95% CI: 28.8-38.9) with enzalutamide alone.
REASSURE: Long-term Safety From a Real-world Observational Study of Radium-223 in mCRPC
Tanya B. Dorff, MD:
With radioligand exposure expected in the bone marrow, we worry about whether treatment with the alpha emitter radium-223 in the setting of bone metastases might lead patients to suffer from a diminished bone marrow reserve. Data from a real-world, observational, long-term safety analysis (REASSURE study) looked at this very question.26
The REASSURE study previously reported that AEs of interest, including serious AEs and drug-related AEs within ≤30 days after radium-223 completion, grade 3/4 hematologic AEs ≤6 months after last radium-223 dose, and drug-related serious AEs after radium-223 therapy completion occurred in approximately 48% of patients overall. Serious AEs leading to death were seen in 9 (1%) patients treated with radium-223. Posttreatment grade 3/4 hematologic AEs occurring ≤6 months after radium-223 treatment completion were observed in approximately 16% of patients (grade 3: 14%; grade 4: 2%). I think it would also have been useful to determine hematologic toxicity in detail beyond 6 months. Nevertheless, investigators did look at drug-related serious AEs for up to 7 years and they report that the rate of any serious AE was 2% overall and less that 1% resulted in patient deaths.
REASSURE: Hematologic Outcomes and Treatments
Tanya B. Dorff, MD:
Based on the REASSURE trial data, the proportion of patients who required red blood cell transfusions, erythropoiesis-stimulating drugs, and colony stimulating factors with or without previous chemotherapy or with or without subsequent chemotherapy was notably increased with the use of radium-223.
COMRADE: Olaparib + Radium-223 vs Radium-223 Alone in mCRPC With Bone Metastases
Tanya B. Dorff, MD:
Data were presented at the 2025 American Society of Clinical Oncology annual meeting for the randomized phase I/II COMRADE trial evaluating radium-223 in combination with olaparib vs radium-223 alone in patients with progressive mCRPC, with 2 or more bone metastases, and without visceral metastases (n = 133).27 The primary endpoint of the phase II portion of this trial was rPFS. Key secondary endpoints included rPFS by disease extent of bone metastases, previous use of docetaxel, and HRR mutation status.
COMRADE: rPFS (Primary Endpoint)
Tanya B. Dorff, MD:
Results from the COMRADE trial showed that the study met its primary endpoint of improving rPFS in the intention-to-treat population.27 Patients who received radium-223 plus olaparib vs radium-223 alone had prolonged median rPFS (8.9 vs 4.7 months; HR: 0.47; P =.0013). In addition, benefits of the combination vs radium-223 alone were observed in patients with no prior docetaxel (median rPFS: 13.7 vs 5.7 months; HR: 0.24), with prior docetaxel (median rPFS: 6.6 vs 3.3 months; HR: 0.73), and equal or fewer than 20 bone metastases (median rPFS: 13.4 vs 4.2 months; HR: 0.21), but not for those with more than 20 bone metastases (median rPFS: 4.7 vs 4.8 months; HR: 1.17). With regard to rPFS outcomes by mutation status, a benefit was observed in patients with HRR-negative status (median rPFS: 11.5 vs 4.5 months (HR: 0.49; 90% CI: 0.34-0.71) but not for those with HRR-positive status (median rPFS: 5.5 vs 4.7 months; HR: 0.47).
Key Ongoing Trials Assessing Radium-223 in mCRPC
Tanya B. Dorff, MD:
Ongoing trials for radium-223 include:
Phase III VISION: 177Lu-PSMA-617 + SoC vs SoC Alone
Tanya B. Dorff, MD:
The phase III VISION trial evaluated 177Lu-PSMA-617 radioligand therapy plus protocol‑defined SoC (defined as either a second ARPI, radiation therapy, dexamethasone, or supportive care, and excluded chemotherapy, immunotherapy, systemic radioisotopes, and investigational drugs) compared with the same SoC in patients with mCRPC.2 VISION enrolled patients with previous ARPI and who also had received 1 or more previous taxane chemotherapy regimen. Patients had to have an Eastern Cooperative Oncology Group performance status of 2 or less as well as adequate organ and bone marrow function. Patients were selected for 177Lu-PSMA-617 radioligand therapy based on visual assessment of PSMA‑PET with diagnostic CT or MRI.3,22 They were randomized 2:1 to receive either 177Lu-PSMA-617 plus SoC vs SoC alone. The coprimary endpoints of the study were rPFS and OS. Key secondary endpoints included objective response, disease control rate, and time to symptomatic skeletal event.
VISION: Efficacy of 177Lu-PSMA-617 + Best SoC in mCRPC
Tanya B. Dorff, MD:
Based on the results from VISION, we saw that addition of 177Lu-PSMA-617 to SoC prolonged OS vs giving SoC alone (median OS: 15.3 vs 11.3 months; HR: 0.62; 95% CI: 0.52-0.74; P <.001). This was equivalent to a 38% reduction in the risk of death from mCRPC. The benefit of 177Lu-PSMA-617 was noticed early on with the Kaplan-Meier curves beginning to separate at 2-3 months after the start of therapy and remaining parallel until after more than 2 years of follow-up.
The coprimary endpoint of rPFS was also improved with a median rPFS of 8.7 months for 177Lu-PSMA-617 plus SoC compared with 3.4 months with SoC alone (HR: 0.40; 99.2% CI: 0.29-0.57; P <.001). The rPFS benefit of adding 177Lu-PSMA-617 to SoC was noted early after starting treatment (approximately 3 months) and it was maintained until approximately 1.5 years.
We know that mCRPC remains incurable for even the population of men with the better prognosis. Nonetheless, the VISION trial showed a benefit with a 60% reduction in the risk of progression or death seen with the addition of 177Lu-PSMA-617 to SoC leading to its FDA approval in March of 2022 for patients with PSMA-positive mCRPC who had previously been treated with ARPI and taxane-based chemotherapy.3
PSMAfore: 177Lu-PSMA-617 vs ARPI in Taxane-Naive PSMA+ mCRPC
Tanya B. Dorff, MD:
Until recently 177Lu-PSMA-617 was available only after docetaxel chemotherapy. There were a few select cases where we considered using it before taxane chemotherapy. For instance, if a patient was ineligible for or was a poor candidate for taxane chemotherapy (ie, good PSMA expression and not too rapid/symptomatic progression, not neuroendocrine histology).
Interest in moving radioligand therapies earlier in the treatment of mCRPC led to the initiation of the phase III PSMAfore trial evaluating earlier use of 177Lu-PSMA-617 vs switching ARPI (to abiraterone or enzalutamide) in patients who had a PSMA-positive lesion (per VISION criteria), had no exclusionary PSMA-negative lesions, had mCRPC progressing on previous ARPI, had not yet received taxanes, and who were not candidates for a PARP inhibitor (n = 468).28 The primary endpoint of PSMAfore was rPFS per Blinded Independent Review Committee (BICR) by RECIST v1.1. Secondary endpoints included OS, rPFS2, and PFS as assessed by the investigator.
PSMAfore: rPFS and OS
Tanya B. Dorff, MD:
PSMAfore met its primary endpoint of improving rPFS by BICR. When compared with an ARPI therapy switch, treatment with 177Lu-PSMA-617 radioligand therapy significantly prolonged median rPFS (11.6 vs 5.6 months; HR: 0.49; 95% CI: 0.39-0.61) including in patients who had not received previous taxane therapy. By contrast, the secondary endpoint of OS in the intention-to-treat population was not improved with median OS being similar for both treatment arms (median OS: 23.66 vs 23.85; HR: 0.98; 95% CI: 0.75-1.26; P = .44).
Based on data from PSMAfore, on March 28, 2025, the FDA expanded the indication for 177Lu-PSMA-617 radioligand therapy to include adults with PSMA-positive mCRPC who have been treated with ARPI therapy and are considered appropriate to delay taxane-based chemotherapy.3
Key Ongoing Trials Assessing 177Lu-PSMA-617 in mCRPC
Tanya B. Dorff, MD:
Ongoing trials for 177Lu-PSMA-617 include:
NCCN Guidelines: Recommended Treatment of mCRPC
Tanya B. Dorff, MD:
The most recent National Comprehensive Cancer Network (NCCN) guideline recommendations list 177Lu-PSMA-617radioligand therapy including for patients with previous hormone therapy (eg, ARPI) and no prior docetaxel if mCRPC and PSMA-positive, as well as for those who previously received ARPI and docetaxel if PSMA-positive metastatic disease is present.7 By contrast, radium-223 plus enzalutamide is recommended for patients with bone metastases in the setting of previous ARPI and/or irrespective of prior ARPI or previous docetaxel for symptomatic, bone-predominant metastases.
Mechanism of Action of 177Lu-PNT2002
Tanya B. Dorff, MD:
177Lu-PNT2002 (also known as zadavotide guraxetan) is another PSMA-targeted small molecule radioligand therapy linked to a DOTAGA radiometal chelator, a bifunctional chelating agent that binds radiometals to form stable complexes via a functionalized glutamic acid moiety which allows it to attach to other molecules including antibodies or peptides via its carboxylic acid groups. It is also designed to specifically deliver radiation to prostate cancer cells.29
SPLASH: 177Lu-PNT2002 vs ARPI in mCRPC
Tanya B. Dorff, MD:
The international, open-label, randomized phase III SPLASH trial evaluated 177Lu-PNT2002 at a dose of 6.8 GBq (±10%) every 8 weeks for up to 4 cycles compared to treatment with abiraterone or enzalutamide in 468 patients with taxane-naive mCRPC progressing on previous ARPI therapy and confirmed to have PSMA-positive metastases via PET/CT with no exclusionary PET-negative lesions.29 Patients also were ineligible for a PARP inhibitor. The primary endpoint of the study was rPFS per BICR per RECIST v1.1. Key secondary endpoints included OS, rPFS2, and PFS by investigator.
What I found most interesting about the SPLASH study is that it explored radioligand therapy every 8 weeks, whereas 177Lu-PSMA-617 radioligand is given every 6 weeks. It also adds to the body of evidence that these radioligand treatments are safe and effective in patients who have not previously received docetaxel.
SPLASH: Primary Analysis of rPFS (Primary Endpoint)
Tanya B. Dorff, MD:
As presented at the European Society of Medical Oncology meeting in 2024, treatment with 177Lu-PNT2002 led to improved median rPFS (9.5 vs 6.0 months; HR: 0.71; 95% CI: 0.55-0.92; P = .0088). OS remained immature at the time of that analysis. With regards to tumor response, we also saw improved best ORR rate (38.1% vs 12%) and median duration of response (9.4 vs 7.3 months).
In a press release, the manufacturer of 177Lu-PNT2002 indicated it would not continue development of this agent due to subsequent analysis showing that it did not improve OS.
ECLIPSE: 177Lu-PSMA-I&T vs SoC in mCRPC
Tanya B. Dorff, MD:
The international randomized phase III ECLIPSE trial is exploring a radioligand therapy known as 177Lu-PSMA-I&T in a similar population of 439 patients with progressive mCRPC who were previously treated with ARPI in the setting of hormone-sensitive or castration resistant-disease. In this study patients are randomized to either 177Lu-PSMA-I&T 7.4 GBq (200 mCi/mL) (± 10%) intravenously every 6 weeks for up to 6 cycles compared with ARPI hormone therapy switch to either abiraterone or enzalutamide (NCT05204927). The primary endpoint of this trial is rPFS. Key secondary endpoints include OS, PFS, PSA response, QoL, and safety.
A press release for the ECLIPSE clinical trial indicated the study had met its primary endpoint of improving rPFS in patients with mCRPC compared with hormonal therapy. We are still awaiting presentation of this data at an upcoming congress.
Other Targeted Radionuclide Therapeutic Approaches Under Investigation in mCRPC
Tanya B. Dorff, MD:
Additional studies are evaluating other radioisotopes as therapy for mCRPC like the alpha-emitter actinium 225 (225Ac), a man-made radioisotope with an approximately 10-day half-life, under development as the active radioligand in various prostate cancer studies.
These studies include:
Integrating Radioligand Therapy Into Patient Care
Tanya B. Dorff, MD:
Now that we have covered the therapeutic landscape for mCRPC, with in-depth insights on the available and emerging radioligand therapies including recent data updates, we can move on to discuss how to integrate these treatments into everyday practice.
There are at least 5 recurrent themes that come to mind when thinking about integrating radioligand therapies into the clinic for mCRPC. These include:
I believe these are all key for the successful application of radioligand therapy in the most beneficial way for patients with mCRPC.
Selecting Appropriate Patients For Radioligand Therapy
Tanya B. Dorff, MD:
The selection of appropriate patients for radioligand therapy can be complex and often involves ensuring that the patient is not eligible for available biomarker-driven therapy such as BRCA/HRR-mutation (Palb2) status or MSI-H/dMMR status—which is often a smaller group of patients. After excluding for potential molecular biomarker–driven therapy, a patient who previously received ARPI and who wishes to delay or has already received docetaxel with mCRPC would be a good candidate for 177Lu-PSMA-617 assuming they meet the PSMA-PET imaging criteria.3,7 As discussed previously, in patients with no previous taxane (ie, docetaxel) and who have mCRPC and bone predominant or symptomatic bone metastases, positive bone scan, and no known visceral metastatic disease, radium-223 plus enzalutamide might be an option.7,13
Factors Contributing to Radioligand Therapy Selection
Tanya B. Dorff, MD:
There are 4 key factors I consider when developing a multidisciplinary treatment plan that involves radioligand therapy. These consider the tumor, treatment itself, the patient, and the care team.
It is key for the medical oncologist to be involved in shared decision-making and patient education. It is also important for the patient and HCP to check in to assess whether to continue radioligand therapy with 177Lu-PSMA-617.
At our center, we are fortunate to have a 177Lu-PSMA-617 tumor board. During such meetings, we perform a multidisciplinary assessment as to whether we need to continue treatment with 177Lu-PSMA-617. For most patients, I can make that decision on my own, but complex cases where PSA levels go down but the PET/CT scan does not look better, or vice versa, are when the tumor boards are most helpful to review the imaging with the nuclear medicine physician or radiologist.
Staying Current With Treatment Guidelines and Universal Recommendations
Tanya B. Dorff, MD:
Being current with the latest clinical guidelines7 and clinical societies such as the American Cancer Society, US Preventive Services Task Force on PSA screening, among others is key to be able to educate patients about their choices and to apply the latest recommendations.
Interpreting Response on PSMA-PET and Utility of SPECT
Tanya B. Dorff, MD:
Assessing response in the context of liver metastases is very important and working closely with a radiologist to interpret liver findings is key. I say this because it can be challenging to assess liver metastases because they are not well delineated on results from PSMA-PET/CT without the use of intravenous contrast. As mentioned earlier, the liver does have some uptake of the PSMA radiotracer, and we want to be certain that there are no PSMA-low/nonavid lesions “hiding” within the liver.
I often involve my radiology and nuclear medicine colleagues, and we may perform other types of imaging (MRI, and IV contrast imaging), particularly when we get discordant cases where disease-related pain gets better but the scans look worse, or the pain is not getting better and the scan does look better. In those scenarios, it is crucial to have the crosstalk between radiation oncology, nuclear medicine, and the medical oncologist.
Phillip H. Kuo, MD, PhD, FACR:
Single photon emission computer tomography (SPECT) is a technique that uses a radioactive tracer like 177-Lu labeled PSMA to help detect recurrent prostate cancer. 177Lu is also a good imaging agent for SPECT. Although less sensitive than PSMA PET/CT, it can also be used to monitor treatment effectiveness and inform personalized therapy in mCRPC cases by providing another useful biomarker to integrate with other biomarkers and clinical assessment.
There might be some variability about how often (after which cycles) to use SPECT/CT given variability in scanner availability. We might consider it in a situation where we suspect that the PSA levels are not accurately reflecting the disease burden. In the setting of a rising PSA, SPECT can localize the site of worsening disease; for example, new disease in the liver generally requires a change of therapy. Use of SPECT in that setting can help assess if the drug adequately reaches and is retained in the tumors. I also think that optimizing the use and interpretation of SPECT/CT is an unmet need and more education and research are needed in this area.
A substudy of the VISION trial mandated by the FDA looked at quantitative 68Ga-PSMA-11 PET parameters using artificial intelligence and semiautomated manual segmentation to determine if there was a correlation between quantitative PET parameters such as whole-body tumor mean standardized uptake value (SUVmean) and patient outcomes.30 The underpinning concept is that tumors with higher uptake on PSMA-PET have higher PSMA target expression and therefore should receive more dose from radioligand therapy and thus are expected to respond better and patients should live longer. We used rPFS as the outcome for tumor response and were able to show that patients with the highest tumor expression of PSMA— for example, lesions with highest uptake of radiotracer— had the longest rPFS. We showed that in the highest uptake quartile of whole body SUV mean ( ≥10.2) in the experimental arm there was a higher rPFS of 14.1 months compared with those in the middle quartiles (≥6.0 to <10.2) 7.8 and 9.8 months and the bottom quartile (<6.0) at 5.8 months. However, I want to make sure that we understand that these quartiles are a function of the distribution of whole body SUV mean in the patient population and do not represent any cutoff that should be used to predict responses. What we do want to emphasize was the finding that the whole-body tumor SUV mean was the best predictor of 177Lu-PSMA-617 efficacy for overall survival and rPFS and it was a linear correlation. In other words, a 1-unit whole-body tumor SUVmean increase was associated with a 12% and 10% decrease in risk of rPFS and death, respectively. Lastly, the pre-therapy PSMA-PET whole body SUV mean is a predictive biomarker for rPFS and OS outcomes since there was a lower hazard ratio in the 177Lu-PSMA-617 plus standard of care arm compared with the standard of care alone control arm.
Although not done in standard clinical practice, the quantification of PSMA-PET scans through segmentation of tumors throughout the body provides proof of concept that the higher the target expression, the better response is going to be.30,31,32 This quantitative imaging biomarker approach for predicting and assessing response is limited to a small fraction of centers currently but should grow.
What we most frequently do in clinical practice is use the visual estimate of high (greater than salivary gland uptake) and low expression with the parameters previously described to help inform which patients are more likely to have better outcomes and thus inform decision-making on whether to use 177Lu-PSMA-617 as the next line of therapy or weighing potential benefits versus risks.
Developing Effective Clinical Care Strategies to Address Associated Risks of Treatment With Radiopharmaceuticals
Tanya B. Dorff, MD:
Aside from doctors who treat head and neck cancers, the management of dry mouth in patients receiving radioligand therapies can be relatively new for medical oncologists. Managing dry mouth is an area in need of optimizing outcomes whereas managing cytopenias is relatively more common to our everyday practice. For the management of dry mouth in patients receiving radioligand therapies, we have had success using pilocarpine, a muscarinic receptor agonist used to increase saliva production, emphasizing good hydration, and dental visits for cavity prevention.
Another important aspect of managing risks with radioligand therapies include dose reduction or dose hold in a patient experiencing myelosuppression or renal toxicity. We may reduce total radiation absorbed from 177Lu-PSMA-617 by encouraging robust oral hydration and frequent bladder voiding.3 Many HCPs are not aware that you can give a lower dose of 177Lu-PSMA-617 if necessary and this is an important point for education.
Phillip H. Kuo, MD, PhD, FACR:
Another consideration is addressing complications around how to manage patients who have nephrostomy tubes or who use disposable undergarments for incontinence. Having a support structure to address AEs and unwanted bystander radiotoxic exposure is of paramount importance.
In patients who have incontinence issues, we educate about how to dispose of items contaminated with “radioactive urine” or any other solid waste (ie, wearing gloves when handling items of clothing or waste, placing them in a plastic bag with a label for description of contents and the date when it was collected, and storing and disposing of waste after decay to minimal to no radioactivity present).
Tanya B. Dorff, MD:
Ultimately patients with mCRPC will have their disease relapse. In patients that relapse while on or after 177Lu-PSMA-617, we do serial PSA testing and imaging based on both PSA and clinical features. I often consider them for trials using the actinium-225 radioisotope-based agent if they previously had a good response to the 177Lu-PSMA-617 radioligand therapy and are now starting to have disease recurrence that remains PSMA positive. Patients with disease relapse for whom a clinical trial might not be an option will move on to receive chemotherapy (ie, docetaxel or cabazitaxel).
The field of mCRPC management is rapidly evolving. Novel radioligand therapy options have changed the treatment landscape with recent indication expansion and emerging ongoing clinical research necessitating more education of HCPs on this topic. By integrating all of the available therapy options and identifying patients eligible for radioligand therapy, we are most likely to empower patients to make the most out of the treatment options available to them to prolong their disease-free and OS.